What is a flexible spending account vs health savings account? FSAs and HSAs are tax-advantaged accounts that help you save on healthcare expenses by letting you use pre-tax dollars. Here’s a quick breakdown to understand:
- Flexible Spending Account (FSA): Set up by employers, these accounts allow you to save pre-tax dollars for medical costs, but with a “use-it-or-lose-it” restriction by year-end.
- Health Savings Account (HSA): Linked with high-deductible health plans, HSAs let you carry over unused funds year after year, allowing for long-term savings and even investment opportunities.
Navigating through the maze of healthcare expenses can be daunting, but choosing between these accounts can lighten the load. Both FSAs and HSAs offer tax advantages, helping small to medium-sized business owners manage healthcare costs while safeguarding their employees’ well-being. Crucially, understanding the difference can significantly impact your financial health.
I’m Les Perlson, experienced in solveing the complexities of health insurance for clients. My insights into what is a flexible spending account vs health savings account draw from years in the industry, ensuring you have clear guidance on these crucial topics.

What is a Flexible Spending Account vs Health Savings Account?
Understanding the difference between an FSA and an HSA is crucial for making informed decisions about managing healthcare expenses. Both accounts offer tax-advantaged ways to pay for medical costs, but they operate quite differently.
Flexible Spending Account (FSA)
An FSA is an employer-sponsored plan that allows you to set aside pre-tax dollars for qualified medical expenses. These expenses can include deductibles, copayments, and even some over-the-counter medications. By using pre-tax funds, you effectively reduce your taxable income, which can lead to significant tax savings.
However, FSAs come with a “use-it-or-lose-it” rule. Any money left in the account at the end of the year is forfeited, although some plans may offer a short grace period or allow a small amount to carry over.
- Employer-Sponsored: Your employer sets up and owns the FSA.
- Pre-Tax Contributions: Contributions are deducted from your salary before taxes.
- Use-It-Or-Lose-It: Funds must be used within the plan year, or they are lost.

Health Savings Account (HSA)
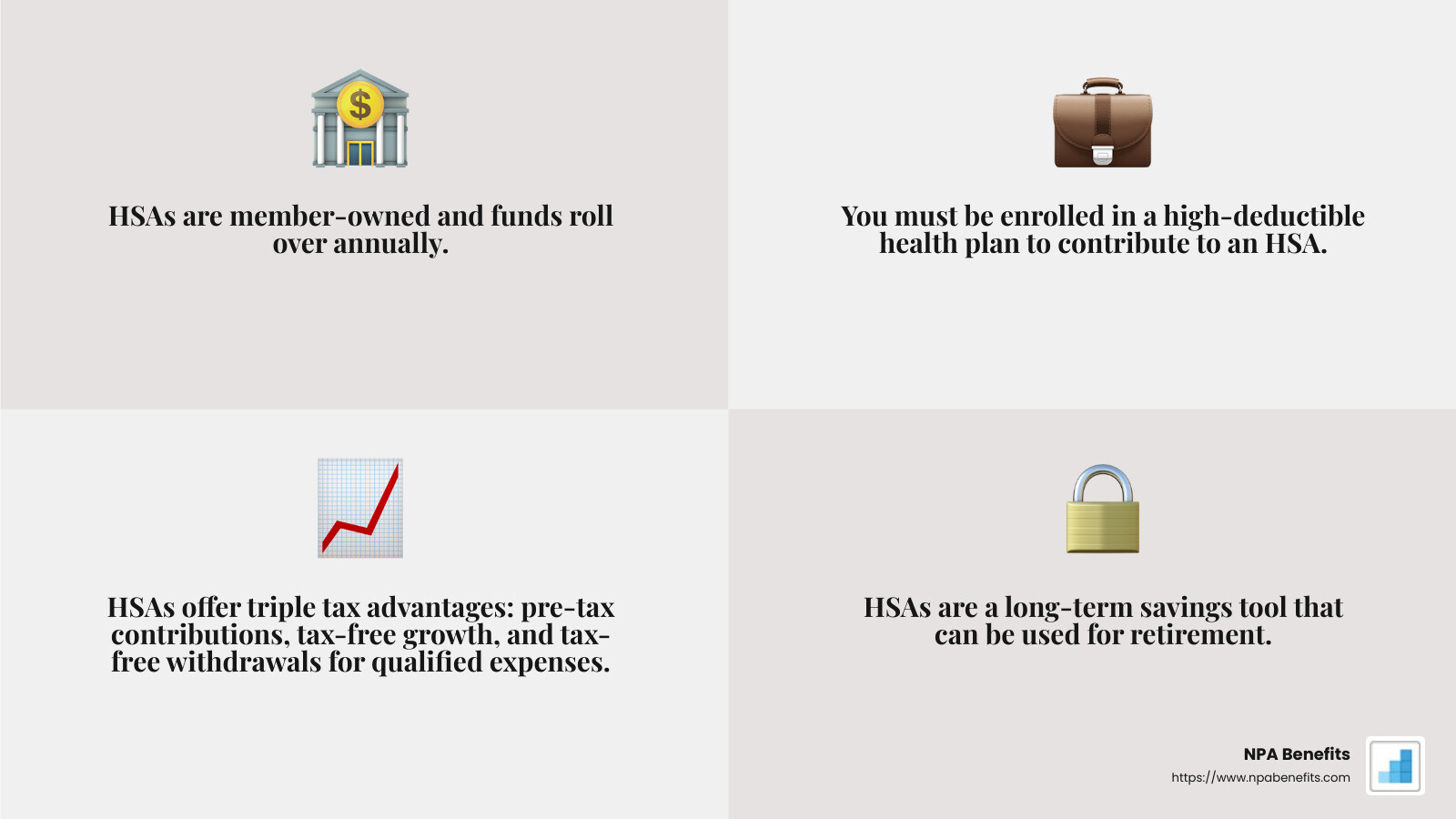
An HSA is a personal savings account meant for those enrolled in high-deductible health plans (HDHPs). Unlike FSAs, HSAs are member-owned, meaning you control the account and its funds. This account is designed for long-term savings, as any unused funds roll over each year and can be invested to grow over time.
HSAs provide a triple tax advantage: contributions are made pre-tax, the money grows tax-free, and withdrawals for qualified medical expenses are also tax-free. This makes HSAs a powerful tool for both current medical expenses and future savings, including retirement.
- Member-Owned: You own the HSA, and it stays with you, even if you change jobs.
- High-Deductible Health Plans: Must be enrolled in an HDHP to contribute.
- Long-Term Savings: Funds roll over annually and can be invested.
Choosing between an FSA and an HSA depends on your healthcare needs, financial goals, and employment situation. Understanding these key features will help you decide which account aligns best with your circumstances.
Key Differences Between FSAs and HSAs
When comparing FSAs and HSAs, understand the major differences in how they’re structured. These differences can significantly impact your financial planning and healthcare decisions.
Contribution Flexibility
Annual Maximums and Limits
Both FSAs and HSAs have annual contribution limits set by the IRS. For 2024, the FSA contribution limit is $3,200. In contrast, HSAs allow for higher contributions: $4,150 for individual coverage and $8,300 for family coverage. This means HSAs might be more suitable if you anticipate higher medical expenses.
Changing Contributions
FSAs are less flexible when it comes to changing your contribution amount. Once you set your contribution at the beginning of the year, you generally can’t change it unless you experience a qualifying life event, like marriage or the birth of a child. On the other hand, HSAs allow you to adjust your contributions at any time during the year, giving you more control over your savings.
Portability and Ownership
Employer vs. Member-Owned
Ownership is a crucial difference. FSAs are owned by your employer, meaning if you change jobs, any unused funds typically revert to the employer. In contrast, HSAs are owned by you, the account holder. This means your HSA stays with you regardless of job changes, offering more stability and control over your healthcare savings.
Job Changes and Retirement
FSAs are tied to your employment and are not portable. If you leave your job, you lose access to any unused funds. HSAs, however, are portable. They stay with you as you transition between jobs or into retirement. This portability makes HSAs a valuable tool for long-term healthcare savings.
Carryover Rules and Investment Options
Carryover Rules
FSAs generally follow a “use-it-or-lose-it” policy, meaning you must use the funds within the plan year or risk losing them. Some employers may offer a grace period or allow a small carryover amount, but these options can be limited. HSAs, however, have no such restrictions. Unused funds roll over from year to year, allowing you to build a substantial healthcare nest egg over time.
Investment Opportunities
HSAs offer the unique advantage of investment opportunities. Once you reach a certain balance, you can invest your HSA funds in various financial products, similar to a 401(k) or IRA. This potential for growth can significantly improve your savings. FSAs, on the other hand, do not allow investments, limiting their potential for long-term financial growth.
Understanding these key differences between FSAs and HSAs can help you make an informed decision about which account is right for you. Whether you prioritize flexibility, portability, or investment potential, knowing these distinctions is crucial for effective healthcare planning.
Pros and Cons of FSAs and HSAs
When deciding between an FSA and an HSA, weigh their pros and cons. Understanding these can help you make the best choice for your healthcare savings and financial goals.
Pros of FSAs
Immediate Access
One major advantage of FSAs is the ability to access your full annual contribution amount at the start of the year. This means if you have a big medical expense early on, you don’t have to wait for funds to accumulate.
Tax Savings
Like HSAs, FSAs allow you to contribute pre-tax dollars, reducing your taxable income. This can lead to significant tax savings, especially if you’re in a higher tax bracket.
Employer Contributions
Some employers may choose to contribute to your FSA. This can provide additional funds for your medical expenses, further enhancing the value of this account.
Use-It-Or-Lose-It
However, FSAs come with a significant drawback. Typically, any unused funds at the end of the year are forfeited. While some plans offer a grace period or allow a small carryover, it’s important to plan your expenses carefully to avoid losing money.
Pros of HSAs
Funds Rollover
Unlike FSAs, any unused funds in an HSA roll over year after year. This can help you build substantial savings over time, which is especially beneficial for future healthcare costs.
Investment Potential
HSAs offer the unique ability to invest your funds, similar to a retirement account like a 401(k). This investment potential can lead to significant growth, turning your HSA into a powerful financial tool.
Retirement Savings
HSAs can be a valuable part of your retirement strategy. Once you turn 65, you can use HSA funds for non-medical expenses without a penalty, although you’ll pay taxes on those withdrawals. This flexibility makes HSAs an attractive option for long-term savings.
Tax Advantages
HSAs provide a triple tax advantage: contributions are tax-deductible, earnings grow tax-free, and withdrawals for qualified medical expenses are tax-free. This can lead to substantial savings over time.
In summary, both FSAs and HSAs offer unique benefits and drawbacks. FSAs are great for immediate access and employer contributions, while HSAs shine in long-term savings and investment growth. Your choice will depend on your healthcare needs and financial goals.
Next, we’ll dive into some frequently asked questions about FSAs and HSAs to further clarify these options and help you make an informed decision.
Frequently Asked Questions about FSAs and HSAs
What is true of a Flexible Spending Account but not a Health Savings Account?
Use-It-Or-Lose-It Policy
One key feature of a Flexible Spending Account (FSA) is the use-it-or-lose-it rule. This means any funds you don’t spend by the end of the year (or grace period, if your employer offers one) are forfeited. In contrast, Health Savings Accounts (HSAs) allow you to roll over unused funds year after year.
Employer Ownership
FSAs are employer-owned accounts. If you change jobs, you lose access to any remaining FSA funds. HSAs, on the other hand, are owned by the individual, meaning the account stays with you even if you switch employers.
Immediate Fund Access
With an FSA, you have access to your entire annual contribution amount at the start of the year. This is like having a line of credit for your medical expenses. HSAs only allow you to spend what you’ve already contributed.
Which is better: a Health Savings Account or Flexible Spending Account?
The answer depends on your personal situation and needs. Here are some points to consider:
Health Savings Account (HSA)
-
Long-Term Savings: If you’re looking for a way to save for future medical expenses, an HSA is better. The funds roll over, and you can invest them for growth.
-
High-Deductible Health Plans (HDHP): You must have an HDHP to qualify for an HSA. This could mean higher out-of-pocket costs if you have frequent medical needs.
-
Triple Tax Advantage: HSAs offer tax-deductible contributions, tax-free growth, and tax-free withdrawals for qualified expenses.
Flexible Spending Account (FSA)
-
Immediate Access: If you anticipate significant medical expenses within the year, an FSA is advantageous because you can access the full contribution amount at the beginning.
-
Employer Contributions: Some employers contribute to FSAs, providing extra funds for healthcare costs.
-
No HDHP Requirement: FSAs don’t require a specific type of health plan, making them more accessible.
Can you have both an HSA and FSA?
Yes, but with some limitations. You can only have a Limited Purpose FSA (LPFSA) alongside an HSA. An LPFSA covers expenses like dental and vision care, allowing you to maximize your savings strategy.
You cannot contribute to a general-purpose FSA and an HSA in the same year. However, you can still have a Dependent Care FSA for childcare expenses without affecting your HSA eligibility.
By understanding these differences, you can better steer your options and choose the right combination for your healthcare savings.
Conclusion
Navigating healthcare savings can seem daunting, but understanding the differences between Flexible Spending Accounts (FSAs) and Health Savings Accounts (HSAs) is crucial for making informed decisions. At NPA Benefits, we specialize in helping you find the best options for your healthcare needs, ensuring you have the resources to make smart choices.
Our goal is to empower you with the knowledge to maximize your healthcare savings. Whether you’re considering an FSA for its immediate access to funds or an HSA for its long-term savings potential, it’s important to weigh the pros and cons based on your unique situation. An FSA can offer tax savings and employer contributions, while an HSA provides investment opportunities and funds that roll over year after year.
Choosing between these accounts often depends on your healthcare needs and financial goals. By analyzing your current and future medical expenses, you can decide which account—or combination of accounts—fits you best.
For more personalized advice and comprehensive solutions custom to your needs, explore our health insurance benefits services. Let us help you achieve peace of mind and financial security, ensuring that you’re well-prepared for whatever healthcare needs may arise.






